Abstract
Background: Non-severe hemophilia A and B account for 50% of patients with hemophilia, in which factor level does not consistently correlate with bleeding phenotype. Clinical decision-making in regards to timely prophylaxis initiation and tailored surgical management could be informed by a biomarker that is more predictive of bleeding phenotype. We hypothesized that a global method to assess clotting potential, such as thrombin generation (TG), is more predictive of bleeding phenotype than factor level.
Objectives: Determine the ability of TG, as compared to standard baseline factor activity, to differentiate bleeding phenotype severity in patients with non-severe hemophilia.
Methods: Subjects were recruited from two hemophilia treatment centers (HTCs): Rady Children's Hospital San Diego (RCHSD) and Center for Inherited Blood Disorders (CIBD). Subjects were eligible for enrollment if they were at least one year of age and had a diagnosis of non-severe congenital hemophilia A or B, or were genetically confirmed or suspected female carriers. All enrolled patients or their parents completed the standardized, self-administered pediatric bleeding questionnaire (Self-PBQ) or bleeding assessment tool (Self-BAT). Clinical and laboratory information were extracted from the medical chart, including age at diagnosis, bleeding event history, past surgical history, treatment history and factor VIII or IX gene analysis.
Validation of self-reported bleeding symptoms was performed using chart-derived data. Bleeding phenotype was assessed using standard calculation of the bleeding score, as defined by the respective validated self-reported tools. For the purpose of this analysis, we defined a high bleeding score as 13 or more, while a low bleeding score was defined as 12 or less. After a washout period of 5x the standard half-life of the administered factor product, blood samples were collected at time of enrollment. Platelet poor plasma was obtained according to a strict protocol to minimize pre-analytical variables. TG was measured by means of the calibrated automated thrombogram, with three different reagents: low (1 pM of tissue factor [TF]), regular (5 pM of TF) and High (20 pM of TF). The following TG parameters were evaluated: Peak TG (Peak), estimated thrombin potential (ETP) and velocity index (VI).
Results: Eighty-one subjects were enrolled. The median age of our cohort was 15.6 years (IQR 21.2, range 4.9 - 59.8), with a slight female predominance (51%) due to inclusion of female carriers. The median follow-up period at the HTC was 5.3 years (IQR 7.5 years), with the majority having follow-up for at least three years. Enrolled patients had the following diagnoses: mild hemophilia A (70%), mild hemophilia B (3%), moderate hemophilia A (13%), moderate hemophilia B (3%), hemophilia A carriers with normal factor VIII levels (10%) and hemophilia B carriers with normal factor IX levels (1%). Median age at diagnosis was 8 years (IQR 26.3, range 0.1 - 56.1), which strongly correlated lower baseline factor activity (r=0.573, p-value < 0.0001). The median baseline factor activity was 21% (IQR 26, range 2 - 249). Factor exposure occurred in 46% of patients (n=37), of which 5 patients were on prophylaxis at time of enrollment. Chronic arthropathy was present in 2 patients (one with mild hemophilia A and one with moderate hemophilia A) and none of the patients had a history of an inhibitor.
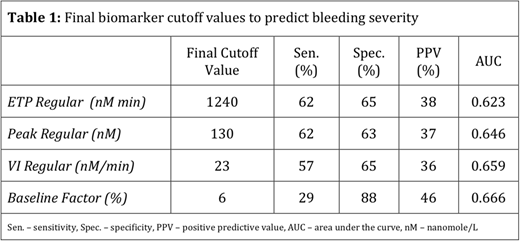
The majority of patients had a low bleeding score (74% vs. 26%). Baseline factor level and TG values obtained with regular reagent (5 pM of TF) showed significant correlation with bleeding score (r = -0.229 to -0.237, p-value < 0.05), while values obtained with other reagents did not show a significant correlation. Sensitivity/specificity analysis revealed the following optimal cutoff values for differentiating between bleeding severities, as obtained from TG with regular reagent: ETP (<1240 nM min), Peak (<130 nM) and VI (<23 nM/min), with analysis results as shown in Table 1.
Conclusion: Even though both TG and baseline factor level had comparable correlation with bleeding severity, all TG values with 5 pM TF showed a much higher sensitivity outcome and greater ability to differentiate between bleeding severities in this population. This approach shows potential for predicting bleeding severity in patients with non-severe hemophilia and should be validated in long-term prospective studies.
Nossair:Novo Nordisk: Other: Conference - Haemophilia Acadamy; Novo Nordisk: Research Funding. Hwang:BPI: Consultancy; Bayer: Consultancy; Hema Biologics: Consultancy; Shire: Consultancy; Bioverativ: Other: PI in clinical research study. Thornburg:ATHN: Research Funding; Bayer Pharmaceuticals: Research Funding; Biomarin: Consultancy; CSL Behring: Research Funding; Bioverativ: Consultancy; Genentech: Speakers Bureau; Octapharma: Research Funding; NovoNordisk: Research Funding; Shire: Research Funding; Johns Hopkins All Children's Hospital: Research Funding; Bluebird Bio: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal